 Sleep apnea is very common in marfan syndrome. See a sleep specialist for diagnosis and treatment. JR
Sleep apnea is very common in marfan syndrome. See a sleep specialist for diagnosis and treatment. JR| Pulmonary Management |
Pulmonary issues are not a major criteria for people with Marfan syndrome however many people with Marfan syndrome have serious pulmonary symptoms such pneumothorax, restrictive lung diseases, chest wall deformaties and sleep apnea.
- Is it possible to confuse lung symptoms of Marfan syndrome with asthma and incorrectly make an asthma diagnosis?
- What are the pulmonary function tests needed to evaluate lung function In people with Marfan syndrome?
- What is the appropriate management of restrictive lung disease? Is it different for people with Marfan syndrome?
- Is there a recommendation regarding chemical versus mechanical scarring for the treatment of repeated collapsed lungs (spontaneous pneumothorax)?
Because fibrillin is expressed in the lung and is associated with elastin there, it is thought to affect both lung development and homeostasis. One possible effect of fibrillin-1 deficiency is pneumothorax. The symptoms of this are shortness of breath, dry cough or an acute onset of pleuritic chest pain. People with Marfan syndrome are at-risk of pneumothorax although they might not smoke. For them, it can be recurrent, present in both lungs and frequently associated with emphysema.
"Small" pneumothorax is treated in the hospital with supplemental oxygen. “Moderate to large” pneumothorax is treated by chest tube evacuation and possibly pleurodesis if necessary.
Restrictive lung disease occurs in more than 70 percent of people with Marfan syndrome. Often, this is due to severe pectus abnormalities and/or scoliosis. In either case, the result is that the chest cannot expand fully. The primary symptom is shortness of breath during exertion.
Emphysema, which results from loss of alveolar walls and enlargement of the air spaces, causes airway obstruction and inflammation. Approximately 10-15 percent of people with Marfan syndrome have emphysema, but it is probably under-diagnosed. It is the structural predisposition of the lungs in people with Marfan syndrome that is probably to blame. Symptoms include shortness of breath during activity, frequent bronchitis (often as a result of common colds or viruses settling in the chest) and low blood oxygen. The diagnosis can be confirmed by a chest x-ray, CT scan, pulmonary function test or arterial blood test. The conventional treatment for emphysema is supplemental oxygen, bronchodilator and aggressive treatment of infections. Research is underway on other pharmaceutical agents that may be useful.
Asthma, which is very common in the general population, is also present in the Marfan community. Respiratory specialists should coordinate care with the other Marfan specialists because the conventional treatments for asthma (beta-agonists) have the opposite effect of beta-blockers which are prescribed to many people with Marfan syndrome.
Pectus deformaties can influence pulmonary function. While surgery can correct the pectus, there is no evidence that pulmonary function will improve. Scoliosis is typically corrected early, but it can be progressive and cause more problems with pulmonary restriction. Serial pulmonary function tests can determine the progress of the lung restriction. Lung dysfunction can be worse if another airway disease, such as asthma or emphysema, is present. Supplemental oxygen and pulmonary rehabilitation are recommended to improve the quality of life.
Some people with Marfan syndrome have sleep apnea, which can have a number of causes. One seems to be laxity of the connective tissues of the airways, which then further relax during sleep and cause partial obstruction to air flow. Often persons with sleep apnea are overweight, but thin persons with Marfan syndrome are also at risk.
Is it possible to confuse lung symptoms of Marfan syndrome with asthma and incorrectly makde an asthma diagnosis?This is often a problem because people who are first diagnosed with Marfan syndrome are frequently children or young adults, an age group in which asthma is a common cause of shortness of breath. Making the correct diagnosis of asthma or another lung problem is important because the beta blocker medication often prescribed to minimize aortic enlargement in people with Marfan syndrome may complicate asthma treatment or make the asthma worse. If the asthma diagnosis is questionable, other explanations for the shortness of breath should be explored.
What are the pulmonary function tests needed to evaluate lung function in people with Marfan syndrome?In order to rule out asthma, emphysema and restrictive lung disease, people should typically have tests including: routine spirometry with and without bronchodilators, lung volume measurements and a diffusing capacity study. If asthma is a strong possibility, provocative testing should be performed. If there is any evidence of restrictive lung disease, maximal inspiratory and expiratory flows should be tested. When sleep apnea is a concern, measurement of upper airway resistance during sleep is a required part of any study for a person with Marfan syndrome.
What is the appropriate management of restrictive lung disease? Is it difference for people with Marfan syndrome?Restrictive lung disease is an inability of the lung to expand adequately in order to take in a full breath. This can be caused by either structural abnormalities of the thoracic cage, such as pectus abnormalities or scoliosis, weak respiratory muscles or lung scarring. For people with Marfan syndrome, the most common causes are chest wall structure or function. Lung scarring is unusual in people with Marfan syndrome. Therefore, the first task for the physician is to determine whether it is a skeletal, muscle or lung problem. This can be accomplished with appropriate pulmonary function testing and a chest CT. Unfortunately, sometimes the degree of restriction does not correlate with the extent of breathlessness or functional impairment. Additionally, apart from early correction of scoliosis, which does improve respiratory function, other surgical measures to normalize the dimensions of the thoracic cage do not always help. Thus, choices about interventions should be individualized to address cosmetic and functional concerns.
Is there a recommendation regarding chemical versus mechanical scarring for the treatment of repeated spontaneous pneumothorax?Physicians who care for people with Marfan syndrome should assume that all patients will eventually require aortic replacement. Therefore, any thoracic procedure should respect the anatomic mandates of future aortic surgery. If supplemental oxygen or chest tube insertion does not successfully treat the pneumothorax, doctors may recommend pleurodesis, which involves "scarring" the lung surface to attach the lung to the chest wall. The best pleurodesis method for individuals with Marfan syndrome is mechanical rather than chemical pleurodesis, as the former makes cardiac surgery easier.
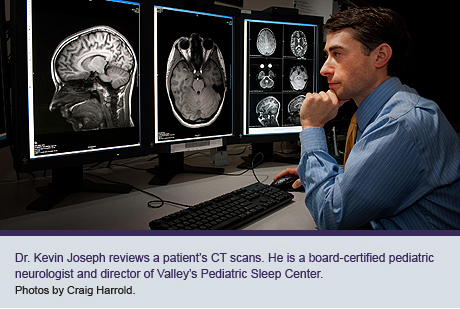 The child displays hallmark behaviors – fidgety, impulsive, irritable, inattentive – and has been diagnosed with ADHD. Dr.
The child displays hallmark behaviors – fidgety, impulsive, irritable, inattentive – and has been diagnosed with ADHD. Dr.  “I saw a boy, 9 years old, who couldn’t sit still in class, couldn’t remember to brush his teeth. Turns out he had severe sleep apnea, like 101 events per hour, and for a child, normal is 1.5 events,” Joseph said. “His oxygen saturations were down in the 70-80 percent level when they should’ve been 95-100 percent. We sent him for a tonsillectomy and at follow-up his parents reported he was sitting in class, not fighting, even losing some weight.
“I saw a boy, 9 years old, who couldn’t sit still in class, couldn’t remember to brush his teeth. Turns out he had severe sleep apnea, like 101 events per hour, and for a child, normal is 1.5 events,” Joseph said. “His oxygen saturations were down in the 70-80 percent level when they should’ve been 95-100 percent. We sent him for a tonsillectomy and at follow-up his parents reported he was sitting in class, not fighting, even losing some weight. Despite well-documented negatives associated with adult sleep disorders, parents are often surprised to learn about sleeplessness’ impact on a child, Joseph said. Sleep is when growth hormone is secreted, fueling body and brain development.
Despite well-documented negatives associated with adult sleep disorders, parents are often surprised to learn about sleeplessness’ impact on a child, Joseph said. Sleep is when growth hormone is secreted, fueling body and brain development.

